Gavin Nielsen was 2 years old when he was diagnosed with a rare and aggressive brain cancer.
The smiley toddler had diffuse intrinsic pontine glioma, or DIPG, a cancer that occurs in the part of the brain stem that controls vital functions including breathing, blood pressure and heart rate. Very few treatment options exist, and the prognosis for children diagnosed with the disease is, on average, less than one year.
“When we have a child newly diagnosed with this disease, we walk into the room and tell the child’s parents their child has a terminal disease and the only option is palliative radiation,” said Dr. Robbie Majzner, director of the pediatric and young adult cancer cell therapy program at Dana-Farber Cancer Institute and Boston Children’s Hospital.
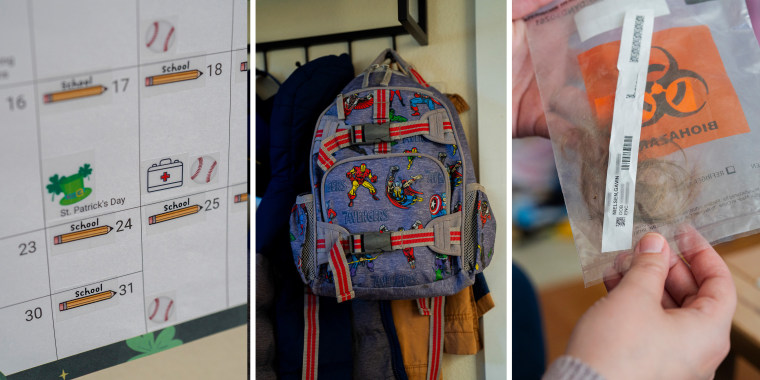
Gavin’s parents started him on radiation. For 30 days, he had to be sedated daily for the treatment. But they also started looking for clinical trials to enroll Gavin in.
At the time, many of the trials for DIPG had a minimum age requirement of 3 years old, his parents, Nate and Ashlee, said.
But Gavin did qualify for one trial, led by Dr. Nicholas Vitanza, a pediatric neuro-oncologist at the Seattle Children’s Hospital Cancer and Blood Disorders Center.
Vitanza is part of a growing group of researchers exploring whether an immunotherapy called CAR-T therapy, or chimeric antigen receptor T-cell therapy, could be effective for treating Gavin’s type of brain cancer. The treatment programs a person’s own T cells — immune cells that usually fight infection — to identify and attack proteins found on tumor cells.

CAR-T has been used to treat certain blood cancers for two decades and got its first Food and Drug Administration approval in 2017. In recent years, doctors have been exploring the treatment in solid tumors, including those in the brain, where patients have few options.
Gavin enrolled in Vitanza’s trial before his third birthday, after he had already completed his radiation treatment.
Doctors started by extracting T cells from Gavin’s blood. Those cells were then modified in a lab to go after the tumor target, called B7-H3. About a month later, he started getting infusions of the T cells, delivered directly into his cerebrospinal fluid. Once reintroduced back into the body, the T cells replicate, creating a surge of cancer-fighting immune cells.

The results of Vitanza’s early-stage clinical trial were published in Nature Medicine in January. In addition to Gavin, 20 children and young adults with DIPG got CAR-T therapy every two to four weeks. The median survival was about 20 months — nearly double the expected prognosis. Three patients, however, are still alive 3 ½ to 4 ½ years after starting their treatment.
Gavin is one of those patients. Now 6 years old, he’s lived four times longer than doctors initially predicted.
“It’s the biggest miracle that I could ever ask for, just to have time,” Ashlee said.
Gavin is still getting CAR-T infusions every two to three weeks. Sometimes, for about 12 hours after the infusions, he has headaches, nausea and vomiting. Other times, he’s ready to run around on the soccer field.
Dr. Mark Souweidane, director of pediatric neurosurgery at Weill Cornell Medicine and NewYork-Presbyterian Hospital, who wasn’t involved with the trial, said the results were encouraging, but added that it’s not “out of the realm of the norm” to have some patients survive longer.
“There are going to be outliers. You will get 5% to 10% of kids who live beyond two years,” he said.
Souweidane said more trials will need to confirm whether CAR-T therapy is, indeed, the reason Gavin and the two other patients in the trial are living much longer than expected. If so, doctors will need to understand whether the therapy could be this effective for everyone with the disease.

“I’m cautiously optimistic that this at least shows some efficacy we can build on in the future,” said Dr. Patrick Grogan, a neuro-oncologist at the Moffitt Cancer Center in Florida. “Until there is a Phase 3 clinical trial with a control group that gets the current standard of care, or robust data from a Phase 2 trial, I tend to take results with a grain of salt.”
Brain tumors present unique hurdles
While CAR-T therapy can be highly effective for certain blood cancers like leukemia and lymphoma, scientists are still in the beginning stages of understanding whether the treatment can be used for solid tumors, which make up the majority of cancers.
“This is entirely experimental,” Vitanza said.

The reason CAR-T therapy works so well in certain blood cancers is because these cancers tend to be homogeneous, meaning their tumor cells are uniform. This gives the immune cells a clear target to latch onto. That’s not the case for solid tumors, which tend to have many different cell types that often differ within individual tumors.
The proteins found in abundance on solid-tumor cells also usually aren’t unique to cancer cells, meaning modified CAR-T cells will also attack healthy cells that have the same target proteins.
“It’s very difficult to find a target specifically on the surface of cancer but not on any tissue,” said Majzner. The goal, he said, is to find a target that’s found in much higher numbers on cancer cells than on healthy cells.

The nonuniform nature of solid tumors means it’s also possible many cancer cells will go undetected by CAR-T cells.
“If you happen to go after a target that is only expressed in 50% of cells, you may have an effect against those 50% of cells but the rest are spared,” Grogan said.
Treating anything in the brain presents additional challenges. The brain is surrounded by a difficult-to-penetrate barrier called the blood-brain barrier, which blocks toxins from entering.
In their trial, Vitanza and his team opted to deliver the modified cells directly into the cerebrospinal fluid, in part to bypass the blood-brain barrier. This also ensured a high concentration of the modified T cells ended up in the cancerous part of the brain rather than in other parts of the body, possibly blunting the number of healthy cells the modified cells come into contact with.

The goal of Phase 1 clinical trials like this is to show whether a therapy shows promise and appears to be safe.
“When you’re dealing with experimental therapies, especially Phase 1 trials, they’re designed to find what is a safe, tolerable dose. You obviously hope there’s a benefit, but it is impossible to quote any benefit, because you’re learning this in real time,” Vitanza said.
Just one patient out of 21 in Vitanza’s trial had a severe side effect, bleeding in the tumor.

Several other early CAR-T trials for DIPG are happening at cancer centers across the U.S. While many questions remain, experts said they are cautiously optimistic the therapy could become a badly needed treatment for DIPG. Kids like Gavin are a crucial piece of the research.
“One thing I always think of is it’s not just Gavin, it’s those kids coming after him, that we’ve met along the way, that didn’t get this chance,” his father, Nate, said. “I think it’s for those kids that we continue.”


