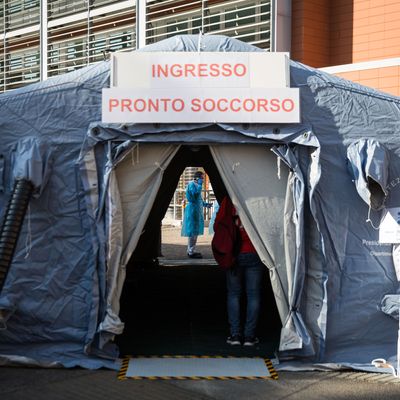
In Italy, where the government reported 475 deaths on Wednesday alone, doctors in hospitals overrun with coronavirus patients have been forced to practice “disaster medicine” and enact battlefield triage to determine which cases receive treatment. “If you are 85, I give the bed to another one who is 45,” Dr. Fabiano Di Marco, the head of the respiratory unit in a hospital in the hard-hit northern city of Bergamo, told the New York Times. “It’s difficult to tell people that if you are 80, you will never have the ICU bed.”
As cases in the U.S. expand rapidly — jumping over 25 percent between Tuesday and Wednesday — state governments and health agencies are now starting to estimate what triage could look like in America, where there is a desperate need for ventilators, the machines that help keep those with severe respiratory inflammation alive. According to NBC News, states are now revisiting care-rationing guidelines put in place after Hurricane Katrina — when a doctor at Memorial Medical Center notoriously hastened the deaths of several patients, leading to second-degree murder charges that were eventually expunged. Known as “crisis standards of care,” plans drafted in at least 36 states help guide health workers in times of profound stress and demand.
In Michigan, the guidelines suggest hospitals could prioritize care and access to ICU beds and ventilators for those performing “essential social functions” — like doctors, nurses, police, military members, and firefighters. In Minnesota, the guidelines detail the determinations doctors must take to decide if patients should be placed on a ventilator, including likelihood of death and underlying conditions. In a crisis, palliative care “may be the only care that is able to be provided due to the patient’s prognosis and available resources.”
New York’s ventilator guidelines do not prioritize by profession, but do recommend that hospitals list conditions based on “immediate or near-immediate mortality even with aggressive therapy.” Patients would then be ranked according to likelihood of survival and the level that they would benefit from a ventilator. In cases of equal need, age would be used as a tiebreaker. Dr. Patricia Powell, a bioethics director at Montefiore Health System, a major provider in southern New York, told NBC News that “you might not get access to a ventilator if you get a prognosis that no matter what, you probably won’t get better.”
As in all catastrophes, the burden of mortal decision-making is not equal across class lines. As actors and athletes receive prompt testing and treatment for the coronavirus, the New York Times reports that some line-skippers of considerable means are contacting ventilator companies to purchase the much-needed machines directly from the supplier as a “fallback plan in case the American hospital system crumbles.” In his Wednesday address to the nation, the billionaire president — whose administration is still attempting to repeal the Affordable Care Act — did not have a solution to such coronavirus health-care inequities. “Perhaps that’s been the story of life,” he said.
We’re committed to keeping our readers informed.
We’ve removed our paywall from essential coronavirus news stories. Become a subscriber to support our journalists. Subscribe now.