It was a reasonable hope: that in time, the novel coronavirus would steadily evolve to become a less dangerous version of itself. We’ve certainly seen this happen with diseases before, such as the 1918 influenza, which killed millions during its first two years but then mutated into a relatively benign form that still circulates today. Likewise, Omicron, though far more infectious than the variants that preceded it, has proven to be somewhat less deadly on a case-for-case basis. Assuming that trend continues, SARS-CoV-2, the virus which causes COVID-19, is in the process of evolving into a relatively symbiotic companion to the human species.
But that idea is a fantasy, say virologists who study the disease closely. “We’re not going to see that,” says Ravindra Gupta, a microbiologist at the University of Cambridge in the U.K. “It’s factually wrong.” Variants will keep coming, and we have no reason to expect that they’ll be less virulent. They could well be both more transmissible and more deadly than anything we’ve seen so far.
The uncomfortable reality is that COVID-19 just doesn’t operate like diseases that we’ve seen before. When it first turned up, many scientists expected that the virus would evolve in pretty much the same way that plants and animals do, with one ancestor leading to another. That is to say, as the virus replicated itself errors would occur in its genetic code, and some of these mutations would result in more successful reproduction. In time, the virus would gradually change as these mutations accumulated, just as the ancestors of the giraffe gradually got longer and longer necks. And in fact, many viruses do evolve this way. “For a lot of viruses that have circulated with us for a long time, we often see this pattern of what we call ladderlike evolution,” says Emma Hodcroft, an epidemiologist at the University of Bern in Switzerland. “They’ve found their ideal way of living in us, and the changes that you see are small.”
The expectation that SARS-CoV-2 would evolve this way too was blown out of the water when the first major variant of concern, later designated Alpha, emerged in the U.K. in September 2020. It wasn’t related to any of the main SARS-CoV-2 lineages then circulating. The same thing happened soon after, when Beta turned up. And again with Gamma. And then again with Delta, and then Omicron. “None of the variants of concern have led to the next variants of concern,” says Hodcroft.
So where did they come from? To understand, it helps to know how coronavirus evolution works.
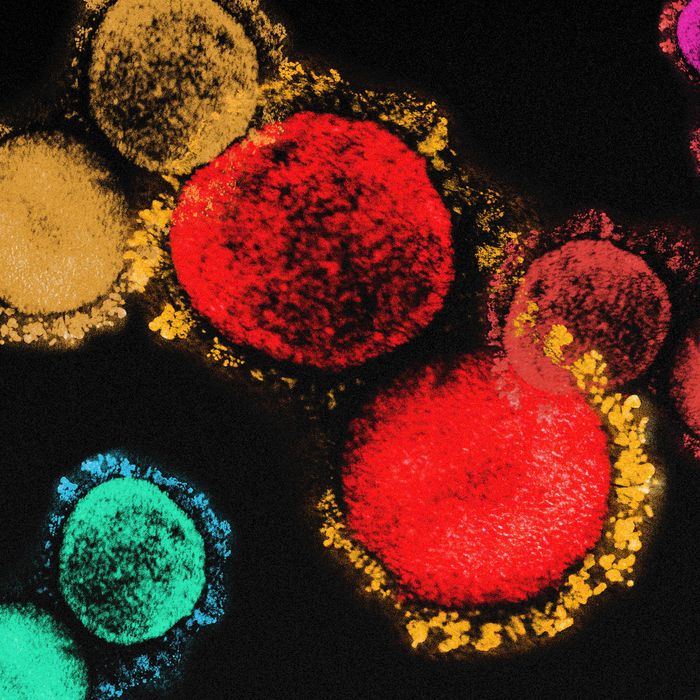
The virus’s genetic code consists of a chain of units called base pairs. Once the virus makes its way inside an infected cell, these base pairs can be read in sequence to produce a few dozen proteins, some of which form its coat. The most important of these is the so-called spike protein, which is crucial in enabling virus particles to infect future hosts.
When a mutation occurs in the spike protein RNA, it can lead to a different amino acid being substituted into the protein, and as a result the spike protein has a better or worse fit with the cell’s surface protein. Mutations elsewhere in the RNA likewise lead to other kinds of changes.
If we imagine all of the possible variations that could happen to the virus genome, we can arrange them onto a sort of virtual landscape in which the elevation represents how good a particular version of the virus is at replicating and spreading, with very transmissible versions as peaks and bad ones as valleys. By definition, any version of the virus that is sitting on a peak is going to be less transmissible if anything about it changes. That makes it harder for the virus to evolve into more infectious versions of itself, but it doesn’t stop it. Says Hodcroft, “The virus can explore a lot of mutation space pretty quickly because it makes literally billions of virus particles in each person, so they can afford to lose a few that don’t work.” By accumulating enough changes to its genetic code, the virus can cross over a valley and ascend another peak — maybe one that turns out to be even higher, just as the Delta variant peak is higher than the Gamma variant peak.
During most infections, the virus can’t explore very far, because it doesn’t have much time. It only takes a couple of weeks for most patients to either defeat the virus or die from the disease it causes. When either happens, replication is shut down.
In fact, if every infection followed this trajectory, then the Alpha, Beta, Gamma, Delta, and Omicron variants never would have arisen. But some infections take a different course. In patients with compromised immune systems, infections can linger indefinitely, with the viral population neither killing the host nor getting killed off themselves. And so the virus has time to explore its mutation space in relative leisure.
Gupta has watched it happen. As described in a Nature paper last year, he and his colleagues observed a patient suffering from persistent COVID-19. The patient was a man in his 70s who had previously suffered from lymphoma. Over the course of 101 days, the team took viral samples 23 times. They found that the virus was continually undergoing mutations, some of which helped the virus evade the host’s immune defenses. As time went by, the different substrains within the patient continuously jostled with one another for dominance. Gupta’s team was witnessing evolution in real time.
Infections like this, Gupta says, are the nurseries of dangerous new variants. And given the scale of the pandemic, nature is churning them out far more effectively than any human lab could. Last year, there was an extended debate in the media over speculation that the original SARS-CoV-2 virus had been created in a facility in Wuhan, China, perhaps as a result of “gain of function” research, in which scientists apply artificial selection to lab-bred strains to try to generate a more transmissible version of an existing virus. Whether or not this actually happened, a similar process goes on naturally inside of the body of every COVID-19 patient suffering a prolonged infection. By the virus’s natural function, it is effectively turning its host into an efficient gain-of-function lab.
A variant’s path to a new peak is a long, elaborate process. Omicron, for instance, contains many changes that accumulated as its ancestor mutated over time. “It takes months, even years, for these viruses to evolve this many mutations,” says Gupta. “We know that immunocompromised people can harbor viruses for more than a year as they keep evolving.”
This, then, is likely where the new variant’s ancestors had been hiding. They hadn’t been wiped out by the later, more transmissible strains because each of them had been lurking inside a patient’s body somewhere. “Omicron is most closely related to viruses that were around in 2020, not even last year,” says Gupta.
As each new wave of COVID-19 sweeps the world, infecting and reinfecting millions, most of the people who are affected aren’t likely to serve as breeding grounds for future variants of concern. But among those infected will be a subset of immunocompromised individuals who will provide that fertile environment. It’s like when a wildfire sweeps across a forest: Once the flames have past, most of the trees are just cold, burnt-out husks, but here and there, pockets of embers remain.
So long as a worldwide population of immunocompromised people exists, the COVID algorithm will continue to run. As long as undiscovered peaks remain to be found, SARS-CoV-2 will continue to find them, jumping from one to the next.
The fact that SARS-CoV-2 jumps instead of creeps is why changes in its virulence have proven so unpredictable. A virus that is only making slight adjustments to a time-tested adaptation will tend to change in steady ways; if it is under selective pressure to become less deadly, it will remain under that same selective pressure and continue to change accordingly. But by jumping radically from one form to another, SARS-CoV-2 is trying out whole new ways of hijacking human cellular machinery. “It’s exploring that in all these different ways and finding different strategies,” Hodcroft says.
While some of these strategies might be less deadly, they could just as easily be more so. And indeed, the variants of concern so far haven’t followed a consistent trend. Alpha turned out to be more virulent than the original strain, and Delta proved deadlier still, but Omicron is less virulent than either — though still about as dangerous as the original.
Even if the next variant to emerge is less virulent than Omicron, that doesn’t suggest that the one after that also will be. Or the one after that. “Natural selection is like a computational algorithm, but one that is not guaranteed to produce a result,” says David Krakauer, a complexity scientist at the Santa Fe Institute in New Mexico. “Every now and then it kicks out an unexpected function.”
One thing that seems likely is that as SARS-CoV-2 continues to explore its mutation space, it will become more and more different from the original variant. Meaning that, as they have for Omicron, the original vaccines will likely become less and less effective for new variants.
So how should all of this inform our response to COVID-19 going forward?
First, to counter the fact that new variants will become ever more dissimilar to the original strain, we need to update our vaccine arsenal. At the moment, we don’t have the technology to rapidly produce new vaccines that specifically target brand-new variants. (Last month Pfizer began testing a vaccine tailored to Omicron just as its wave was starting to retreat.) But by making vaccines that combine proteins from multiple previous variants, we can train our immune systems to recognize viruses from a wider swath of the possible mutation space. “If a new variant appears in a neighborhood that we didn’t know existed yet, there’s not a lot we can do about that,” Hodcroft says, “but if it’s in neighborhoods that we’ve seen before, we’ve got some protection.”
Next, to shut down the virus’s computational power, we need to suppress the waves of infection that leave behind the smoldering stumps. “Stopping chronic infections is going to be a tall order, so obviously the easiest thing to do is to limit the number of total infections,” says Gupta. “This is one of the reasons why global equity on vaccinations is so important.” With a worldwide pandemic, it’s no use just vaccinating ourselves; we have to vaccinate the collective human body, all 7.9 billion individuals.
Eventually, says Hodcroft, the novel coronavirus will stop being so novel; it will have lived with us so long, and caused so many infections, that it will have made all the big leaps that exist for it to make and settled into a quieter sort of middle age marked by slower evolution and less virulence. “I think the question going forward is, ‘When is the virus kind of done?’” she says. “When do we not see variants that are so crazy?”
Unfortunately, she says, we have no idea how long that will take. “We don’t know how many more tricks it might have up the sleeve.”