On April 13, the FDA and CDC recommended that use of Johnson & Johnson’s COVID-19 vaccine be suspended after six women developed serious blood clots after receiving a dose, one of whom died. The CDC will “review these cases and assess their potential significance,” the agencies said in a joint statement. While the cases amounted to less than one per million vaccinations, they resembled similar blood-clot events suffered by recipients of the vaccine made by AstraZeneca, which uses a similar adenovirus vector.
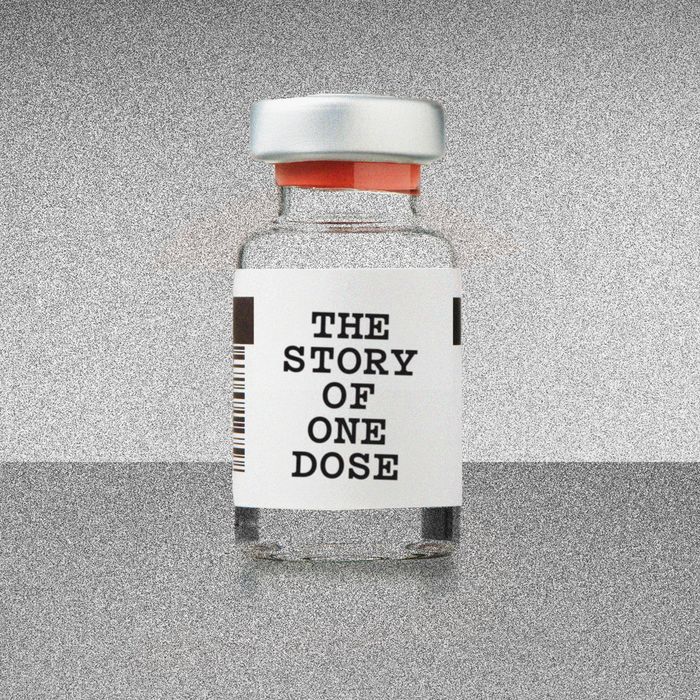
As an object, it’s not much: an inch and a half of glass with a stopper and some liquid inside. But a thimbleful of the stuff has amazing power — the ability to liberate us from our yearlong collective trauma. The fact that it’s available, scarcely a year after the start of a pandemic, is both an industrial miracle and a freakish stroke of luck; a decade ago, technology did not exist that could bring vaccines so quickly to the public’s arms.
Pfizer and Moderna crossed the finish line first, neck and neck, in December. The third and most recently approved vaccine was from Johnson & Johnson. The J&J vaccine holds some crucial advantages: Only one dose is required rather than two, and while the other approved vaccines expire 30 days after thawing, Johnson & Johnson’s lasts three months, making it easier to distribute in countries that lack an advanced cold chain. The story of the vaccine’s path from development to mass distribution is a lesson in the power of the global capitalist system — the network of corporations and supply chains that, though it can suffocate and disempower us as individuals, can also summon forth immense material and intellectual resources and deploy them for the greater good.
From the start, J&J struggled to catch a break. The pharmaceutical giant played it safe during development and lost crucial time, failed to get FDA approval for parts of its U.S. production chain, missed several delivery targets, and wound up with a vaccine that underperformed its rivals in clinical trials. Then, another obstacle: Last week, the New York Times revealed that the new batch J&J had pledged would be delayed even further, after a mix-up at a subcontractor’s production facility ruined 15 million doses. The Biden administration has since directed J&J to take over every aspect of vaccine production at the plant.
The setback was significant, but not fatal. The facility where the mix-up occurred was part of a production process that relies on a precise orchestration of timing, engineering, and logistical expertise across multiple continents, which makes it vulnerable to bad luck and human error. But the system is also resilient: When the batch of J&J doses was compromised, alternative supply lines were available to compensate for the failure. Here is how that entire tempestuous journey unfolded — the breakthroughs, the setbacks, and the way the pieces came together to bring vaccines to millions of arms.
1.
Sequencing
On the afternoon of January 3, 2020, a box arrived at the laboratory of the Shanghai Public Health Clinical Center, a complex 30 miles southwest of the city center. The box contained swabs taken from a patient in Wuhan who had fallen ill with a new kind of pneumonia. Worried about how dangerous the new pathogen might turn out to be, the Chinese government had banned medical researchers from publishing any information about it. China had experienced public-health scares before: Between 2002 and 2004, a deadly and highly infectious virus called SARS had spread through the country. It was in response to SARS that the Shanghai Public Health Clinical Center had been built.
Zhang Yongzhen, the laboratory’s leader, was a specialist in assessing new viruses. Over the next 40 hours, his team painstakingly broke the genetic code of the new pathogen into its sequence of nucleotide base pairs — essentially decoding the software that the virus plugged into its host to make copies of itself. The sequence would tell researchers exactly how it worked so that they could figure out how to thwart it.
At 2 a.m. on January 5, according to a profile in Nature, one of Zhang’s team members gave him bad news: The virus was a close relative of SARS. Though little was yet known about how the disease progressed or how it was transmitted, the potential for rapid spread and widespread death was real.
On the morning of Saturday, January 11, Zhang was on a plane about to take off for Beijing when he got a call from Edward Holmes, a virologist from the University of Sydney. Holmes, a longtime colleague of Zhang’s, knew that he had sequenced the virus’s genome. Holmes impressed upon his colleague the importance of publishing the information. Zhang asked for time to think. If the new disease was as contagious as SARS, it could spread beyond China and put the whole world at risk. But there was a more immediate hazard: the danger of angering Chinese authorities. An airline attendant appeared and told Zhang that the flight was about to take off. He had to decide. “Okay,” Zhang said. Holmes could release the sequence data.
2.
Planning
In Boston, on the other side of the international dateline, it was still Friday, January 10. Dan Barouch, a virologist at the Beth Israel Deaconess Medical Center, was hosting an off-site meeting with his lab at the Boston Museum of Science, in a room that enjoyed a view of the Charles River. Barouch and his team had gathered to plan for the year ahead, but everyone was discussing the news from China, where the first death linked to a new form of pneumonia had just been announced. “It had all the hallmarks of a virus that we thought might have pandemic potential,” Barouch recalls.
In some ways, this was the moment Barouch had been preparing for. For the last decade and a half, he and his team had been developing a “vector” — a way to sneak part of a pathogen’s genetic code into human cells. Once there, it would trigger the cells to create pieces of the pathogen for the body’s immune system to identify. Their vector was a variant of an adenovirus, a bug that causes the common cold. Called Ad26, it had had several of its genes removed so that, while it was able to insert itself into human cells, it couldn’t reproduce and make a person sick. But it could still merge with the human host cell and bring with it the pathogen DNA needed to cue the immune system. This approach could theoretically work with almost any infectious agent — Barouch’s team had already used Ad26 to make vaccines for HIV, tuberculosis, and Zika. Pfizer and Moderna would follow a similar technique using mRNA; by using DNA, a more stable nucleic acid, Barouch & Co. were crafting a vaccine that could be injected in one dose.
It was Friday evening, Boston time, when Zhang’s data hit the internet. Zhang’s lab had decoded the virus into letters symbolizing the four base pairs that make up its genetic code: A, C, G, and T. In effect, Zhang and his team had compressed a living thing into pure information. By uploading it, they had transformed it again, into a string of ones and zeros split up into packets that bounced around the fiber-optic nodes of the internet. Barouch and his team went to work. On Monday, they began translating Zhang’s digital data back into nucleotide sequences, which, in turn, could be converted back into an actual virus. It was as though pieces of the coronavirus had teleported through the web.
Immediately, Barouch saw the best strategy. He noticed that the virus contained a spike protein — a piece that sticks out like the rubber hair on a Koosh ball, which an antibody in the human bloodstream would be most likely to recognize. From the genome, Barouch could tell which stretch of DNA coded for it. To make the vaccine, this would be the sequence to pack into the Ad26 vector. The question was what exactly the message should contain: the whole spike protein sequence or just part? Should the scientists include a preamble, or other sections that might help get the message across to the immune system? The decision could mean the difference between an efficacious vaccine and a useless one.
Meanwhile, the disease was spreading rapidly in China and cases were starting to appear internationally. Barouch contacted Johan Van Hoof, the head of vaccine development at Janssen Pharmaceuticals, a subsidiary of Johnson & Johnson with R&D centers in Leiden, the Netherlands. They had worked together on vaccine development for more than a decade. “Johann, this is looking bad,” Barouch told him. “I think we need to make a vaccine.”
“Absolutely,” Van Hoof said. “We do.”
3.
Assembling
The labs in Boston and Leiden began working in parallel, staying in touch with daily phone calls. They started by creating a dozen different lengths of DNA and injecting them directly into mice to see which triggered the most vigorous immune response. They then winnowed the list to seven candidates, packed them into the Ad26 vector, and tested the variants on Rhesus monkeys. It was a bit like A/B testing of different versions of an Internet ad: Each version of the DNA snippet would cause the body’s cells to produce a different protein, which, in turn, would have a different effect on the immune system. They wanted to make sure they chose the most powerful one.
On February 11, the worldwide death toll passed 1,100, with more than 44,000 cases reported in China and several other countries. Health officials at last gave the disease a name: COVID-19. In those crucial early months, every day in the lab presented an existential battle between quality and speed. If Barouch and Van Hoof made a best guess at the right sequence and put it straight into the vector, they could roll out the vaccine sooner and save countless lives — the approach that Moderna and AstraZeneca chose. But this could result in an inferior vaccine that would allow more people to die. In the end, the scientists decided to take a few months to test multiple versions on animals first, then advance the most effective one to human testing.
They ran the test on 52 animals. Some of the variants were given to four animals, others to six. The researchers then exposed all the test animals to COVID. Compared to control animals, the monkeys that received versions of the vaccine showed little viral replication. But monkeys that received a variant called S.PP showed almost no sign of infection at all. On March 30, 2020, it was this variant that Janssen announced as its vaccine candidate. It was called Ad26.COV2.S.
To ensure that the Ad26.COV2.S would be safe and effective for humans, the company would need to test it — first on a few hundred people, then on tens of thousands. It normally takes years to conduct a full slate of tests, get results, and design a follow-up round. Instead, Van Hoof’s team began running steps in parallel. As soon as it could see what direction the animal tests were going, the lab started to produce vaccine material for human trials — a decision that would move the trial start date up from September to July. And, in April, even before the results of the clinical trial came in, Johnson & Johnson began making plans to manufacture and package the vaccine at scale, so that mass quantities would be ready by the time the human tests came back. If the results were good, J&J could quickly start putting needles in arms. If not, the vaccines would get chucked in the trash, and billions of dollars spent on research and development would go up in smoke.
Months later, Johnson & Johnson learned it had made the right call. Clinical-trial results showed the vaccine worked and was safe, and it received a green light from the FDA in February 2021.
4.
Manufacturing Substance
Johnson & Johnson makes a wide variety of medications, but it had never fulfilled an order as large as the coronavirus vaccine, a drug that 7.8 billion people — 331 million in the U.S. alone — needed right away. By spring, the Trump administration was lobbing contracts at vaccine-makers: $483 million to Moderna, $456 million to Johnson & Johnson, $30 million to Sanofi, then $1.2 billion to AstraZeneca, and $1.95 billion to Pfizer. Johnson & Johnson promised 100 million doses, but even that was way beyond its capabilities. So to augment production from Janssen’s own facility in Leiden, it signed up partners around the world to produce its as-yet-unproven vaccine, including, in the U.S., a company called Emergent BioSolutions.
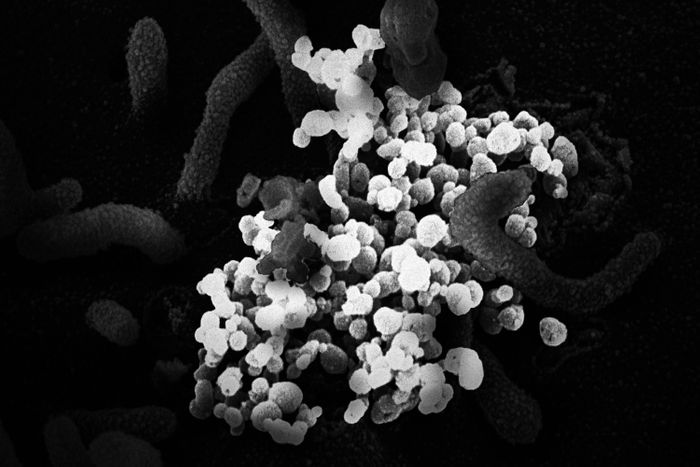
Founded in 1998 to produce anthrax vaccine as a defense against terror attacks, Emergent had, over the years, received hundreds of millions of dollars to provide doses for the U.S. government’s strategic stockpile. When the threat came in the form of a pandemic, it was tasked, instead, with manufacturing millions of doses of Ad26.COV2.S. But growing Ad26 viral vectors wasn’t a straightforward process. To turn the original virus into a harmless vaccine, researchers had deleted genes the virus needs for replication; in order to make copies of itself, the Ad26.COV2.S vector required a special environment. The solution was to insert the virus’s missing genes into a unique human-cell line that had originated in the eye of a human fetus aborted in the mid-1980s. This genetically modified cell line was named PER.C6. Unlike normal human cells, which can multiply only so many times before dying, these cells are immortal; as long as they’re fed the right nutrients and kept at the right temperature, they can grow forever. Because PER.C6 contained the genes that Ad26 needed to reproduce, it held the key to growing the viral vectors.
Last fall, in an office park in East Baltimore, Emergent technicians added the contents of a cell-culture bag to a ceiling-high tank holding a single-use bioreactor. The bioreactor was filled with a 1,000-liter solution of sugars, proteins, and other nutrients. Inside the warm bath, cells began to multiply.
Once the PER.C6 cells grew to the right volume, workers added several liters of Ad26.COV2.S seed containing millions of vector particles. Inside the bioreactor was a genetically engineered paradise. The adenovirus particles latched onto the exterior of PER.C6 cells and injected them with their DNA. Once inside, the genetic material caused the cells to start manufacturing the components that make up the virus particle, until the hosts were so stuffed with tiny self-assembled machines that they burst, spewing out a conquering robot army into the broth. After a week, the PER.C6 cells were either hijacked or dead, and the tank contained quadrillions of virus particles, enough for millions of doses. Waste and cell fragments got filtered out, and what was left was concentrated, then frozen at 94 degrees below zero. The resulting material is known as vaccine substance.
For months, this process took place again and again in Baltimore and in the Netherlands. But by early 2021, the millions of units of vaccine substance produced at Emergent still weren’t allowed to leave the plant. Like Moderna and Pfizer, J&J, under the pressures of a global crisis, had begun activating parts of its supply chain before all of them had received the official green light, and the FDA had not yet inspected and approved the Baltimore facility, which had, in recent years, received a string of citations for quality-control issues.
Then, in late February, disaster struck. Emergent accidentally mixed Johnson & Johnson vaccine ingredients with those of AstraZeneca’s, destroying 15 million doses and further delaying the facility’s FDA approval and the delivery of more vaccines. The plant had caught the error and quarantined the incorrect doses, and, in the meantime, a new supply line was starting to get under way — in March, President Biden announced that the pharmaceutical giant Merck, which had abandoned its own vaccine initiative, would convert and upgrade its facilities to help manufacture more J&J doses. But until it could sort out the mess, Johnson & Johnson was forced to rely on vaccine substance produced at Janssen’s plant in Leiden.
5.
Creating Product
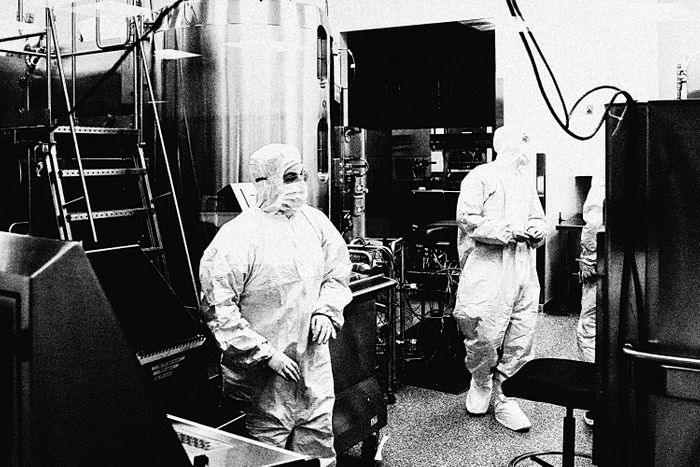
After the vaccine substance is manufactured and approved, it then has to go to a “finish and fill” facility, where the deep-frozen concentrate will get turned into stuff that can actually be injected into a person. Last year, J&J scrambled to contract with Catalent Biologics, an international pharmaceutical processing company that could quickly expand its plant in Bloomington, Indiana. In June, Catalent was also tapped to finish-and-fill the Moderna vaccine.
Inside a space that, a year ago, was an empty warehouse, gleaming panoplies of stainless-steel arms and wheels whir. Behind aseptic barriers, the vaccine substance is thawed, blended with substances like 2-Hydroxypropyl-β-cyclodextrin (to improve its solubility) and Polysorbate 80 (a stabilizer often used in food and cosmetics), then fed into a vial-filling assembly line. Sterilized vials move by conveyor belt into a filling station where a multipronged needle bobs up and down, squirting ten full at a time.
There is no margin for error. A single vial that gets chipped or cracked could ruin an entire production run. Optimizing this kind of process is a never-ending task, with chemists and engineers tuning and tweaking at the nano level. The material sciences company Corning, for instance, recently figured out how to prevent glass from flaking off vials by switching from borosilicate to aluminosilicate, a substance it calls Valor Glass.
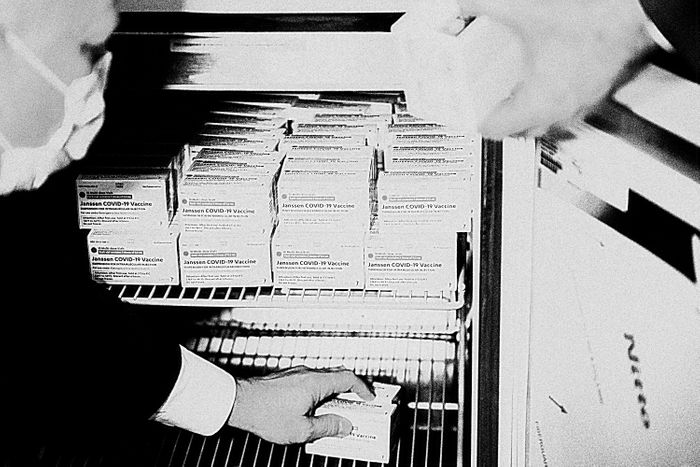
Each newly filled vial contains five doses — about a quarter-trillion adenovirus particles in three milliliters of liquid. A printer lays an alphanumeric code around the vial, then a robotic packing machine places ten vials in a box, at a rate of 600 vials a minute. During the filling process, no human hand has intervened once. As with Emergent, Catalent’s new facility needed an FDA signoff before the material it produces could be released to the public — on March 23, 2021, that approval finally arrived. Five days later, the Bloomington plant began shipping out J&J vials, which could then join the 6 million finished vaccines that had been sent to the U.S. from J&J’s Netherlands factory.
6.
Distribution
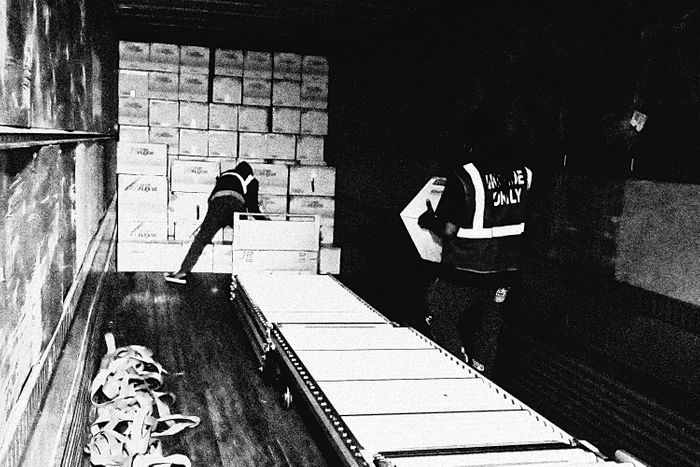
Late last year, a billboard appeared along the highway in Shepherdsville, Kentucky, a rural town 20 miles south of Louisville. “NOW HIRING,” it said. “Material Handlers Get Paid Up to $20.12 Per Hour.” The jobs were posted by McKesson, a large pharmaceutical-distribution company that had been contracted by the Centers for Disease Control and Prevention to package and dispatch all COVID-19 vaccines, except for Pfizer’s. In late 2020, the company completed construction on its brand-new Shepherdsville facility, a squat, quarter-mile-long million-square-foot warehouse, and it needed to hire more than 500 workers.
In the race to create and distribute the vaccine, McKesson’s role may first appear as mundane as that of any fulfillment center: It’s tasked with counting out the correct number of ten vial-size boxes for each site (900 vaccine doses to a high school in Kalamazoo, Michigan, say, or 300 to a health center in Athens, Georgia) and packaging them into cartons for shipment. But it’s the scale of the operation that’s key — a huge portion of America’s vaccine production will, at one point, need to go through McKesson. Its Shepherdsville hub is one of the company’s four facilities shipping COVID vaccine doses; to construct the storage racks alone required at least 3.7 million pounds of steel, more than a quarter of the metal frame used to construct the Eiffel Tower.
Inside a hangar-like room hung with American flags, workers load the boxes of J&J vaccines into KoolTemp EPS coolers, adding frozen gel packs and a monitoring device that logs the temperature and triggers a warning if it gets too high or low. To prevent that from happening, workers are allotted 30 minutes to place the coolers into cartons. (In another section of the facility, Moderna doses, which must be maintained at a lower temperature, are packed inside a freezer by workers wearing parkas and insulated boots.) McKesson workers are also tasked with assembling the kits that contain everything a vaccination center needs to administer the vaccines: alcohol pads, face shields, surgical masks, and needles and syringes.
Less than two days after arriving at the McKesson warehouse, the vaccine is off on the next leg of its journey.
7.
Shipping
A UPS semi pulls up to the loading dock, and workers place the KoolTemp cartons into the trailer. The truck swings onto the onramp to I-65 North and drives the 20 miles to UPS Worldport, a 5.2-million-square-foot intermodal shipping hub located on the grounds of Louisville Muhammad Ali International Airport. There, the boxes are unloaded, scanned, and sorted through a 155-mile-long system of conveyor belts.
Until now, each stage of the vaccine-making process has required some kind of scientific or logistical coup: the compression of a years-long process into a matter of weeks, the creation of a new technology, the rapid alteration of a physical landscape. But when it came time to move those millions of doses to their final destinations, it took barely any extra effort for UPS and FedEx to activate their networks. After all, among the 20 million packages delivered daily, thousands of vaccine shipments were a rounding error.
In 2019, UPS introduced a service for health-care customers that allows them to more precisely track shipments of medicines, samples, and vaccines. Each carton is affixed with a tag that allows sensors to track its location, and the data gets transmitted to the UPS health-care command center inside Worldport, a room with four large-screen monitors on the wall displaying national weather and UPS flights in transit. When bad weather before Christmas meant that a vaccine shipment’s destination was closed, for instance, the health-care command center got on the phone and arranged to have it redirected.
As the cartons wend their way through the maze of conveyor belts, scanners read the label on each and shunt it to the appropriate outbound loading station. Shortly before midnight, planes start arriving at the Louisville airport at the rate of about one a minute, carrying inbound packages; those packages get sorted at the rate of 115 every second, then loaded back onto planes heading for their final destination.
Within 15 minutes of its unloading at Worldport, a box slides down a chute to the outbound station. A worker scans it and checks all six sides for damage, then loads it into an airfreight shipping container bound for New York. Around 4 a.m., the pilot takes off.
8.
Administration
Later that morning, the box arrives at the loading dock of a vaccination site. This final leg of the vaccine’s journey — delivering doses to a place where they can be put into people’s arms — is the simplest in concept, but was, for a long time, the most vexing. In the weeks after the first vaccines were approved and shipped, New York State proved ill-prepared to deliver its allocated doses. By early January, some vaccination sites had used less than 20 percent of the doses they’d been sent.
Similar problems played out across the country. Despite having lavished billions on producing vaccines, the Trump administration had largely ignored the question of distribution and administration, leaving the matter to states and offering little support. Entire organizational structures had to be built on the fly using whatever labor happened to be available. In New York City, the effort leaned heavily on the Medical Reserve Corps, a group of more than 15,000 volunteers who stand by to help out in crises. By the end of January, the system was running smoothly enough that the vaccination centers were efficiently doling out what they’d received.
When it’s your turn, you roll up your sleeve. The nurse chooses a needle based on the heft of your arm — an inch and a half for larger people, an inch otherwise — and pushes the tip into the rubber gasket atop the vial containing your dose. She slips the needle into your muscle. Inside your arm, 50 billion genetically engineered nanoscale robot assassins, carrying genetic payloads downloaded from the internet and bred in a soup of immortal human-eye cells, begin prying their way through your cells’ defenses.
This article was featured in One Great Story, New York’s reading recommendation newsletter. Sign up here to get it nightly: