This article was featured in One Great Story, New York’s reading recommendation newsletter. Sign up here to get it nightly.
One morning at the end of April 2023, Marcela Maus, a cancer researcher at Mass General in Boston, got a call from her colleague Bryan Choi. “He called me, and he’s like, ‘Oh my God, oh my God, oh my God!’ And I’m like, ‘What is going on?’” Maus said. Choi, a neurosurgeon with the languid demeanor of a surfer, was not given to outbursts. Maus hung up the phone and hurried over to his office.
The day before, Choi and Maus had treated their first patient in a clinical trial for an aggressive brain cancer called glioblastoma, infusing genetically modified white blood cells directly into the fluid surrounding the brain. They had been up all night worrying, especially after the patient, a 74-year-old man, developed a fever. Choi had ordered an MRI. “We were not looking for the results,” he said. “We were trying to make sure that our patient was okay.”
When Maus got to Choi’s office, images from the MRI were loading on his screen. They stared in wonder: The patient’s tumor, which a few days before had shown up on the scan as a bright blob the size of a strawberry, had almost entirely disappeared. No one had heard of that kind of regression in glioblastoma, especially not overnight. “My first instinct was that there was something wrong with the MRI scanner,” Choi said. But then the follow-up scans looked even better.
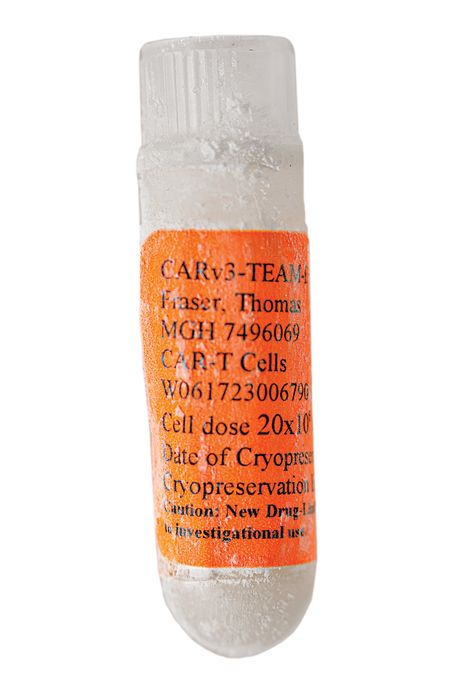
Several weeks later, they treated a second patient, a civil engineer from upstate New York named Tom Fraser, and the process repeated itself: the infusion, the fever, and the rapid regression of the tumor. “It was almost like clockwork,” Maus said, still sounding astonished months later. After a third patient had a similar response, she paused the trial and wrote up her results.
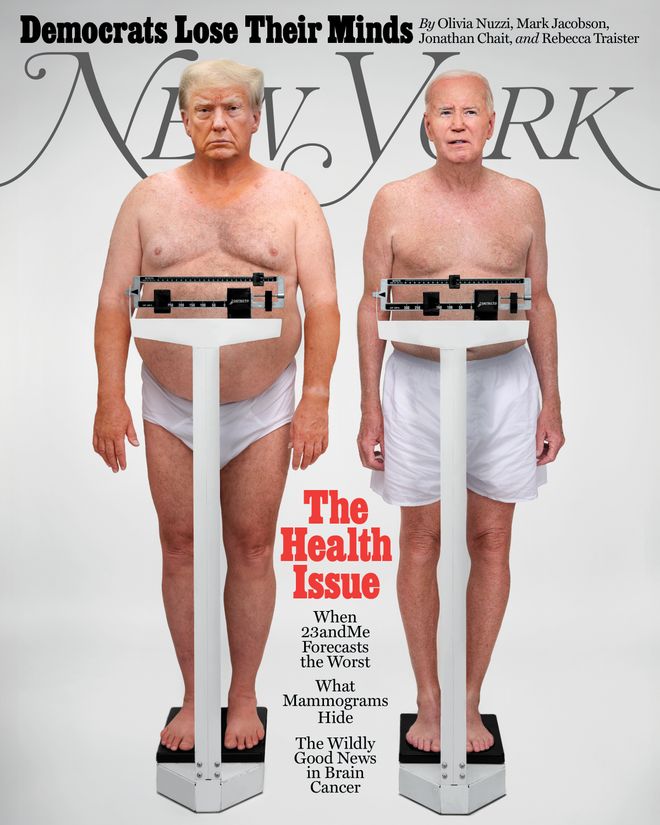
In this Issue
Glioblastoma is the most common type of malignant brain cancer. It can strike at any age, and it’s uniformly fatal. Patients are often diagnosed in the emergency room after the tumor causes some somatic catastrophe, such as seizure, sudden loss of speech, or an inability to control the limbs on one side of the body. The median time from diagnosis to death is just over a year.
The first step in treating the disease hasn’t changed in decades: “maximal safe resection,” a surgery to remove as much of the tumor as possible while preserving neurological function. Because glioblastoma is so adept at infiltrating the brain, the surgeon almost always leaves cancer behind, which quickly starts growing again. Some patients respond to radiation or the chemotherapy drug temozolomide, but even that adds months rather than years to the average survival time. Roger Stupp, an expert in glioblastoma (he wrote the paper that made temozolomide “standard of care”), told me the disease had proved to be “a graveyard of ideas.” Decades of research have gone nowhere.
Within the past 20 years, however, a once unfashionable field called immunotherapy has upended all expectations in oncology. It proceeds from a simple premise: The human immune system is very good at attacking anything it registers as disease. If it could be turned against cancer, it could eliminate a tumor more thoroughly than a surgeon’s knife and more durably than the poison of chemotherapy.
Maus and Choi thought they’d found a way to do just that using the immune system’s all-purpose killer: the T cell, which the body sends to neutralize pathogens of all sorts, including bacteria, viruses, and parasites, but not (usually) cancer. By extracting T cells from a patient’s blood, editing the cells’ DNA in a lab, and reintroducing them at the site of the tumor, they had gotten the body to react to cancer as it would to a virus and destroy it. It was the culmination of years of research in immunotherapy labs like the one Maus runs at Mass General.
Fraser remembers that on the day of his infusion, the room was crowded with doctors, nurses, and scientists. There was a sense, he said, that history was being made. “I felt a little poke when the needle was inserted,” he wrote me in an email, “but it was a very quick process.” Twenty-four days later, he walked out of the hospital, weak and exhausted but with his tumor in near-total remission.
“There’s been a revolution in understanding cancer and the tools to tackle it,” Daniel Haber, the director of the Mass General Cancer Center, told me. Immunotherapy, paired with our greater understanding of the genetics of cancer cells, has produced breakthroughs for previously untreatable forms of the disease, especially in liquid tumors like leukemia and lymphoma and skin cancers like melanoma. Death sentences have been commuted; hopeless cases have been cured.
Until recently, the biggest exception to this parade of good news has been in solid tumors like pancreatic cancer and glioblastoma, which have resisted almost all efforts to check them. So Fraser had it right. If these early results from Boston held, it would make history. If we can treat glioblastoma — perhaps the hardest case in a field made up of hard cases — there’s not a cancer that would seem to be out of reach.
After Choi and Maus published their results in the New England Journal of Medicine in March, they heard from oncologists all over the world. “They’re desperate, and they say, ‘We want to offer something because there’s just nothing out there,’” Choi told me. The status quo, Choi knew from his own patients, was miserable.
This spring, I got to witness the kind of brain surgery that’s standard of care for glioblastoma but may one day become obsolete. It was both simple and high-tech. Five figures in blue scrubs stood around the patient, and there were screens on every wall stacked like amps at a death-metal show. I was led around the operating table, ducking between machines until I arrived at the patient’s head, where the surgeon showed me how he could insert a stereotactic probe and see on the monitor exactly where in the brain he was working.
A square of scalp on the patient’s head was peeled back to reveal the skull underneath. A smaller area of skull, about the size of an eye patch, had been removed, and the brain itself sat exposed, pulsing with each heartbeat, as if it were breathing. And it was: The engine of cognition, the seat of human consciousness, the anthropocentric core of the universe lay before us, and it was alive, fragile and yet somehow bursting with vitality, like it wanted nothing more than to leap free of the vessel that contained it.
On a screen on the far wall, I could see a hole where the tumor had been, an almost perfectly round miniature planet. I switched my gaze to look at the brain directly. The hole was darker than I would have imagined. I tried to stare all the way into its bottom but could see only black.
Patients with glioblastoma are often sent to surgery within days of their diagnosis. The urgency comes both from the aggressiveness of the disease and the unique nature of the brain itself. Trapped inside the skull, there’s nowhere for it to go when a tumor begins growing. As normal tissue is pushed aside, the neurological effects can multiply quickly. Cancer elsewhere in the body can be debilitating, but it’s unlikely to suddenly take away your ability to speak, to move, to think.
Maus and her team started enrolling new trial participants in May. Hundreds of people with glioblastoma have written to or called Mass General about the study, but Maus had room for only 18 more. I asked her whether they had already filled the remaining spots. She said they couldn’t: Until recently, her team could treat only one patient at a time, and the disease progresses too quickly to look more than a few months into the future. “It’s heartbreaking,” Maus said about having to turn people away. “You get a lot of stories.”
Not long ago, I spoke with Katie McKay, whose husband, Kevin, was diagnosed with a brain tumor in 2016. That summer, Katie and Kevin were driving down for a vacation in Myrtle Beach with their two children, ages 3 and 5. They had made good time from their home in Annapolis, so Kevin phoned the hotel and asked if they could check in early. Shortly after he hung up, he began convulsing and moaning. The kids were watching cartoons in the back seat, “and they thought he was playing a joke on them, like being like a monster, and I thought so too,” Katie said. “I grabbed his arm, and I realized his eyes were in the back of his head.”
Katie pulled to the side of the road and Kevin’s head fell in her lap. He was out for several minutes, during which he soiled himself. When he woke up, Katie was standing outside the passenger side of the car checking his pulse. “He’s like, ‘Katie, what are you doing?’ And I said, ‘Nothing, everything’s fine. Something seems a little off with you.’”
At the hospital in Myrtle Beach, doctors saw two lesions on his brain. Kevin had his first surgery on August 2, at Johns Hopkins, and began radiation and chemotherapy. When Katie recounts the months that followed, her voice falters as she remembers how difficult their lives became. She kept spreadsheets of appointments and medications and leads to follow for novel treatments. “I started researching because I remember in the beginning going to a lot of the appointments and not knowing the lingo,” she said. “And I didn’t want to waste any more time asking somebody, ‘Can you tell me what they were talking about?’”
Katie and Kevin were college sweethearts. They met at the University of Maryland and married in 2010. He was so lovable, Katie said. He liked to play little pranks on the family: dropping habanero in Katie’s drink when she wasn’t watching or waking his mother-in-law up with a leaf blower. He was 32 when he was diagnosed.
Kevin remained optimistic even as the disease progressed, while Katie remained, in her words, the worrywart. “In the beginning,” she said, “I would cry and be so sad and have so much anxiety about it, worrying about his fate, and he would be like, ‘Hey, Katie, if not us, it would be somebody else.’” Eventually, he had to step back from his job as an engineer, and Katie had to drive him everywhere while trying to manage the kids’ schedules. She enrolled him in a trial at Johns Hopkins, but it didn’t seem to have much of an effect. He lost the ability to sense his left side. Soon, he could no longer speak.
Kevin died in July 2018, two years after his first seizure. As the tumor spread throughout his brain, he qualified for a trial at MD Anderson Cancer Center, but Katie decided against it: “He was already in a wheelchair. He was in a diaper at that point, and I could not feasibly get him there.” She said she’d rather spend her final weeks with him at home than subject him to a treatment that likely would not work.
When Maus started her Ph.D. in immunology a little more than 25 years ago, the idea that it could one day make brain tumors like Kevin’s disappear was laughable. “I was told that it was career suicide,” Maus said. “People had been trying for a hundred years to get the immune system to recognize cancer, and it was a dead end.”
Maus is short and has an eager smile and dark, expressive eyebrows. When I met her at her lab at Mass General in a building one block from Boston Harbor, I got a sense of how she might have stuck it out despite the warnings from her colleagues. She was friendly but didn’t let me get away with being wrong, a practice seemingly honed from years of supervising Ph.D. students and postdocs. “Let me tweak that,” she would say back to me when I fumbled through a question about cellular biology. Her attraction to immunotherapy was simple: Because it should work, she was determined to make it work.
Maus knew that though cancer has long confounded efforts to kill it, it has a vulnerability. Cancerous tissue can be a pinpoint or a swarm, but it is always made up of cells. And those cells have to be at least somewhat different from the other cells in the body, or they wouldn’t be cancer. If you could train the immune system’s T cells to recognize that difference, that would be the end of the disease.
Efforts to attain that goal have already reshaped oncology. Researchers have developed drugs that selectively bind to proteins in cancer cells, inactivating them (targeted therapies); they’ve discovered ways to attack tumors by modulating the body’s immune response (immune checkpoint inhibitors); and they’ve gotten good at growing white blood cells outside the body and reinfusing them to overwhelm a tumor.
Some of these approaches, while powerful, were a bit like flooding your house to get rid of the rats. What if we could hire an exterminator instead? Immunologists zeroed in on the T cell, learning how to manipulate its genetic code to prompt it to hunt for specific proteins on the surface of cancer cells; other changes made the T cells more active. This engineered T cell has a special name: a CAR-T cell. (car stands for “chimeric antigen receptor.” The receptor is what binds a T cell to a protein on a cell’s surface. Antigen is another name for that protein. And the chimera, in this case, is the hybrid between the T cell’s normal receptor and its genetically modified components.)
A decade ago, when Maus was at the University of Pennsylvania, her mentor, the immunologist Carl June, developed an astonishingly effective CAR-T therapy for leukemia. In some forms of the disease, a class of white blood cells called B cells begins to divide rapidly. June and his team programmed their CAR-T cells to target a protein on the B cells’ surface called CD19.
The CAR-T cells did their job quickly and thoroughly, binding to CD19, eliminating the B cells, and curing the leukemia. Almost overnight, CAR-T cells became the most exciting technology in cancer. Today, more than 34,000 leukemia patients have received some form of CAR-T therapy, and there are some 1,100 different CAR-T trials underway around the world. Everyone working in June’s lab became cancer-world famous. (At a recent conference, a scientist who got up to speak after June told the audience he felt like he was “standing up to play the ukulele after the Rolling Stones.”)
The biggest question in oncology today is whether this approach could also be used for solid tumors. Maus was one of dozens of specialists in immunotherapy who began looking for a suitable cancer for a new CAR-T trial. “I’m not an expert in any disease right now,” she told me, “but I think a lot about how to get T cells to do what we want them to do. The T cell is my hammer, and I’m on the lookout for nails.”
Glioblastoma, she knew, had a promising nail for the T-cell hammer: an antigen called epidermal-growth-factor-receptor variant III (EGFRvIII), which isn’t found in healthy brain tissue. In a clinical trial she began before moving to Mass General, she and a neurosurgeon at Penn named Donald O’Rourke gave patients intravenous injections of T cells engineered to target EGFRvIII.
The experiment was a failure. Some of the CAR-T cells made it to the patients’ brains, but they didn’t seem to have any effect on the tumor. By the time Maus set up her lab at Mass General in 2015, she had two ideas for how to improve the treatment, “one big one and one medium one.” The medium one was to infuse the T cells directly into the fluid surrounding the brain, which would, she hoped, allow more of them to reach the tumor.
The big idea was meant to address a separate problem. Glioblastoma, like most solid tumors, is heterogeneous. Different parts of the tumor have different proteins on the surface of their cells, which makes eliminating them by going after EGFRvIII alone impossible. Maus’s new CAR-T cell was engineered to secrete a molecule called a bispecific T-cell engager, which acted like a bit of double-sided tape, making it easier for T cells to bind to a second protein called wild-type EGFR. The approach, Maus said, was “as fine-tuned as I can possibly imagine.”
Maus and Haber were at dinner when she showed him scans from the first patient. “The world stopped,” he said. The possibilities were immediately clear. “If it’s really working in glioblastoma,” he said, “does that open up the whole bandwidth of solid tumors?”
Maus was quick to point out the limits of what this first phase of the trial has proved. The modified T cells were remarkably effective, but they also eventually disappeared, probably killed by the body’s own immune system. Of the three patients, one died from a perforated bowel, an adverse reaction to a medication he was taking. The second had a recurrence within months of the tumor vanishing. And even Fraser, who had the longest-lasting response, has recently seen signs that his cancer is starting to grow again. “I feel like this was a double or a triple,” Maus told me. “It’s not a home run.”
June’s assessment was more sanguine. He compared Maus’s experiment to his celebrated work with leukemia. It took just five years to get from their first promising results to FDA approval; today, thousands of patients have been effectively cured. “I think by 2029, we’re going to have FDA approval of CAR-T cells for glioblastoma,” he said. “It’s going to be a huge thing, and 2024 is going to be looked at as the breakthrough year.”
Cancer researchers are fluent in the language of failure. The past century, divided in half by Richard Nixon’s declaration of a war on cancer in 1971, has been marked by frustrations and setbacks, approaches that should have worked but didn’t. Oncologists once thought they were treating a single disease. Now they know that no two types of cancer are alike. Indeed, the same cancer in two individuals can be wildly different. “Cancer,” Haber told me, “is as complicated as medicine.”
For all the promise of immunotherapy, there are formidable obstacles. The first of these is cost. At Maus’s lab, every device and every person represents tightly coiled helixes of time and money. There are PCR machines, biosafety cabinets, ELISA readers, autoclaves, freezers, cell counters, incubators, and centrifuges. The proliferation of white, boxy machines makes the space look like an open-floor-plan office with an unusual number of personal mini-fridges.
When I visited, many of the researchers on the floor (there are dozens of them — young, a mix of genders and races) were staring at computers. Others were busy at what we’d recognizably call lab work, transferring liquids from one container to another, moving things in and out of freezers, placing things under a microscope or removing them. The lab itself carries Maus’s affect: friendly but solemn, collegial but not disposed to gossip or chitchat. Nearly everyone has an M.D., a Ph.D., or both.
Maus walked me through some of the steps needed to create CAR-T cells for the trial. We started with the room where the DNA instructions that are added to the T cell’s genome are written. (“I ran my first restriction digest on a DNA plasmid the summer after eighth grade,” Maus told me. “I was so excited. I didn’t sleep for two days afterward.”) We went on to the lentiviral-production room, where technicians create viral vectors carrying this DNA. From there, we moved to the tissue-culture room, where the vector is mixed with normal T cells to create the CAR-T. Finally, we visited the immune-monitoring part of the lab, where lab techs assay blood draws and other samples from patients, looking for proof that the CAR-T cells have made it to their targets.
Maus calls the lab “as whole shebang as you can get.” The only part missing are the mice they use for testing; those are upstairs. Maus says she’s glad of that — she’s allergic to mice. It takes this whole apparatus, working together, weeks to create enough T cells for one infusion.
Jennifer Wargo, a professor of genomic medicine at MD Anderson, referred to the cost of immunotherapy treatments as “financial toxicity.” The patent for June’s CAR-T therapy for leukemia is owned by Novartis, and the median cost for the treatment is $620,000. Even if drug companies don’t try to profit from these therapies, the process is inherently labor-intensive: T cells have to be removed from the patient’s own blood, genetically altered, then reinfused. It’s difficult to determine where economies of scale might kick in.
The complicated process of producing CAR-T cells also limits the number of people who can be treated. For an emerging therapy like CAR-T for glioblastoma, the restrictions are even greater. Over the past few months, I spoke with several patients searching for a trial that would take them on. Michael McNally was diagnosed last summer, after he noticed a slight droop on the left side of his face. He went to Mass General, suspecting a mild stroke. After an MRI, the doctor told him he had a tumor in his right frontal lobe. “I said, ‘Look, we’re changing the rules here at Mass General,’” McNally said. If a doctor delivered news like that, “you better have a Redbreast whiskey in your right hand.” He had surgery two days later.
McNally has gone through an exhaustive list of treatments trying to improve on the standard of care, including a personalized cancer vaccine. “If someone told me scorpion poison would kill it, I’d probably take it,” he said. “I’m a giant mouse; let’s go. Let’s do it.” He won’t be able, however, to enroll in Maus’s trial. Because they want to ensure that any positive outcome can be attributed to the CAR-T regime alone, the exclusion criteria rule out anyone who has been treated with “any prior gene-therapy or gene-modified cellular therapy.”
Timing can be difficult for patients and their families to manage. After her father, Yuriy, was diagnosed with glioblastoma, Yelena Tsyrlin tried to enroll him in an immunotherapy trial right away, but she still missed the eligibility window. (She has since started the process to secure a spot in O’Rourke’s follow-up study to the one he conducted with Maus, which has also shown promising results.) Another caregiver wrote that her mother kept getting rejected from trials because she was still on hormone therapy for breast cancer, which she’d had more than five years earlier. “I understand the reasoning and the science behind these decisions,” she wrote, “but when you’re facing this as a patient or a family member, it feels cruel.”
None of the oncologists I spoke with thought that immunotherapy would completely supplant proven approaches. Some cancers will still be best treated by surgery, others by radiation or chemotherapy. CAR-T therapy may be reserved for the most stubborn cancers.
As more CAR-T treatments get FDA approval, however, cost and efficiency may improve. “You’re on the incipient curve of discovery,” Haber said, “but science builds on itself, and sometimes things that are incredibly complicated, expensive, and dangerous open the door to things that become much more democratic, affordable, and standard.” Researchers are looking at ways to use a virus to genetically modify T cells inside a patient’s body, effectively eliminating half of the steps Maus walked me through in her lab. Others are experimenting with vaccines that can teach the immune system to target the same kind of antigens that the CAR-T cells bind to.
Maus and Choi have already refined the protocol for their glioblastoma trial. Patients will now have a short run of chemotherapy before the infusion to limit the number of CAR-T cells killed or inactivated by the innate immune system, allowing more of them to remain active at the tumor site for longer.
In our first conversation, I asked Maus if Mass General hired her because of the incredible results from the CAR-T therapies developed at Penn. She said they weren’t hiring a CAR-T specialist; they were hiring a T-cell specialist. The difference was meaningful. The CAR-T cell, as complicated as it is, is one expression of a much deeper knowledge. That may be how we ultimately reduce costs: The better we understand the immune system, the easier it will be to find ways to make it do what we want.
On the first day of summer, I went to visit Tom Fraser, participant No. 2 in the trial, at his home outside Rochester. I had been warned that the cancer had made speaking difficult for him, and all my phone communications to that point had been with his wife, Debbie. After spending months talking to patients with glioblastoma and their families, I feared the worst. So it was a pleasant surprise to be greeted at the door by a tall, sturdy man with a shock of salt-and-pepper hair. “Welcome,” he said, shaking my hand. “I’m Tom Fraser.” He led me to his tidy kitchen, where we sat and talked for nearly two hours. The sun outside was almost unbearably bright.
Before he retired, Tom led a forensic engineering firm. After some catastrophe, he’d be called in to determine its causes. When a Bethlehem Steel warehouse near Buffalo caught fire a few years ago, sending up a plume of smoke so large 300 households and several schools had to be evacuated, Tom determined that the culprit was an improperly installed lighting system that had thrown sparks onto flammable materials below.
He takes the same methodical approach to discussing the course of his disease, consulting a timeline he’s marked out on a legal pad. “I put some dates down here just so I can remember,” he told me. Sometimes Debbie, voluble where Tom was laconic, with a neatly trimmed gray bob, would interject. Tom would pause to listen, then return to his outline.
In August 2021, they were staying at their cottage in the Thousand Islands — a little white house perched on a rock in the Saint Lawrence River — when Tom first knew something was wrong. “I got up in the morning,” he said, “and I couldn’t read.” It took him a month to schedule an MRI, but once he did, the diagnosis arrived quickly. He’d never heard of glioblastoma, but his doctor was direct with him: Without treatment, he could die within six months. He and Debbie told their family — four daughters and eight grandchildren — the news over Zoom.
One of Tom’s daughters works as a physician’s assistant at Mass General, and she encouraged him to travel there to get his tumor resected. His surgeon, Brian Nahed, needed nearly five hours to complete the operation. Tom showed me the scar, a horseshoe on the left side of his head. “It’s okay as long as I can comb my hair over it,” he said.
After the surgery, he started radiation and chemotherapy, then underwent treatment by Optune, a device that uses electric fields to try to disrupt cell division. Nahed was frank about the likelihood of any of these approaches keeping the cancer in remission for long. “He said, ‘That’ll work until it doesn’t work,’” Debbie told me. “‘This is what happens. This heterogeneous cancer figures out ways. That’s what makes it so aggressive and so difficult to treat.’” Even so, when the cancer recurred after 20 months, the Frasers felt blindsided.
It was Nahed who suggested Tom enroll in the trial being run by his colleagues at Mass General, calling the Frasers at dinner on a Sunday night in the spring of 2023. His message was one of both caution and hope: There was no guarantee this treatment would work, but there was also no more promising trial anywhere in the world.
On the day of the infusion in July 2023, 30 people crowded into the room with Tom and Debbie to watch. For all the time and money and innovation that went into producing that moment, the scene was oddly humble: a normal hospital room, Tom sitting up in his bed as a doctor wearing gloves pushed the plunger on a syringe.
The next month was difficult. Even though the scans showed the tumor shrinking, matching the dramatic results from the first patient, the doctors were reluctant to read too much into them. “They really were very careful not to give us information, even though we were asking all the time,” Debbie said. In the weeks that followed, Tom suffered a cascade of complications: atrial fibrillation, mysterious infections, a punishing fever. The nurses swaddled him in blanket after blanket, but still he shook uncontrollably. Debbie kept watch 12 hours a day. Choi tried to reassure them that the effects were a sign that the treatment was working.
“By the time I left,” Tom said, “I could hardly walk.” Debbie showed me a picture from that day. Tom looked feeble and miserable, “not himself,” in her words. “Let me see that,” Tom said, and Debbie turned the picture to him. “Oh,” he said. “That is not myself.” When they arrived back in New York, the grandchildren greeted them with a WELCOME HOME poster, a hand-drawn rainbow floating near the bottom.
That fall, Tom felt strong enough to return to the family’s cottage in the Thousand Islands. He wanted to help power-wash the house, but Debbie overruled him. They knew nothing about participants Nos. 1 and 3 in the trial and precious little about Tom’s own prognosis. “We knew that things were stable, but we did not know the profound results,” Debbie said. That all changed when Maus and her team published the paper in the New England Journal of Medicine.
If CAR-T therapy for glioblastoma eventually becomes standard of care — if Maus and others can reproduce and improve on the results she got for Tom Fraser — his name will forever be tied with the birth of this treatment. “I shouldn’t say it, but I’m a little proud of myself,” Tom said. “There were three of us in the group, the first three to ever have it and try it. And I was the No. 2 guy.”
Hope can be a shot of adrenaline or the steady drip of an IV, but it’s always strong medicine. The intense days of those first incredible scans are long behind the Frasers; they have settled into a different rhythm recently, something approximating the way they were before the diagnosis. Tom has also shifted the way he talks about his disease. For years, he spoke about beating glioblastoma — finding a cure for himself. Now he’s more likely to refer to the patients who come after him, who will undoubtedly live longer because of what we’ve learned from his response to the CAR-T therapy. This spring, he packed up his library of engineering reference books and donated them to Clarkson College, his alma mater.
He might not be done with his fight yet, however. After a scan in February showed signs of recurrence, a new set of images taken in June showed just the opposite. The tumor had seemingly shrunk again. “I said, ‘Holy crap, I’m going to do a dance,’” Tom said. Now, according to Debbie, he’s in better shape than he’s been in months. Was it a temporary effect or a sign that the T cells were still active in his brain? We may only know years from now, and then only by implication, if a strong enough signal emerges from future CAR-T trials.
Tom’s next scan is not till August. In the meantime, he told me about a trip he and Debbie were planning: “I’ve never visited Chicago in my life. I said, ‘This is nuts. I want to see this place — so let’s go.’” That morning, they had been to their youngest grandson’s fifth-grade graduation. It was a hot day, and they sat sweating in the parking lot. It had been almost three years since he’d been told he might have six months to live.